Eating for PCOS: Nourishing Your Body with a Non-Diet, HAES-Aligned Approach
Eating for PCOS: a nourishing Non-Diet, HAES-Aligned Approach
Polycystic Ovarian Syndrome (PCOS) is a common hormonal condition affecting around 12–18% of women, though up to 70% may remain undiagnosed. The experience of PCOS is incredibly individual, but common symptoms can include irregular periods, acne, unwanted hair growth, low energy, and emotional changes. These symptoms are often linked to elevated levels of hormones such as testosterone and insulin, which can affect how the ovaries and other body systems function.
At The Wholebeing Co., we take a weight-inclusive and HAES-aligned approach to nutrition care. This guide explores how gentle, evidence-based nutrition can support PCOS symptoms.
What is PCOS?
PCOS is a hormonal condition diagnosed by 2 out of 3 of the following criteria:
1. Higher levels of testosterone in the blood
2. Irregular menstrual cycle
3. Polycystic ovaries (follicles) on ultrasound.
Note: Polycystic ovaries alone are not sufficient for a diagnosis.
Common symptoms of PCOS may include:
Irregular or missing menstrual cycles
Fatigue and low energy
Acne or excess facial/body hair
Weight fluctuations
Anxiety or depression
Difficulty conceiving
Scalp hair thinning (alopecia)
PCOS is a lifelong condition, and symptoms can vary in severity over time. Management may include tailored dietary and lifestyle changes alongside medications or hormonal treatments when necessary.
Insulin Resistance and PCOS: What You Need to Know
Insulin resistance is a common feature of PCOS and can play a role in increasing the risk of conditions like pre-diabetes, type 2 diabetes, and heart health concerns. The good news is that supportive dietary and lifestyle strategies are often the first line of care, and can make a difference in managing insulin resistance
What is Insulin Resistance?
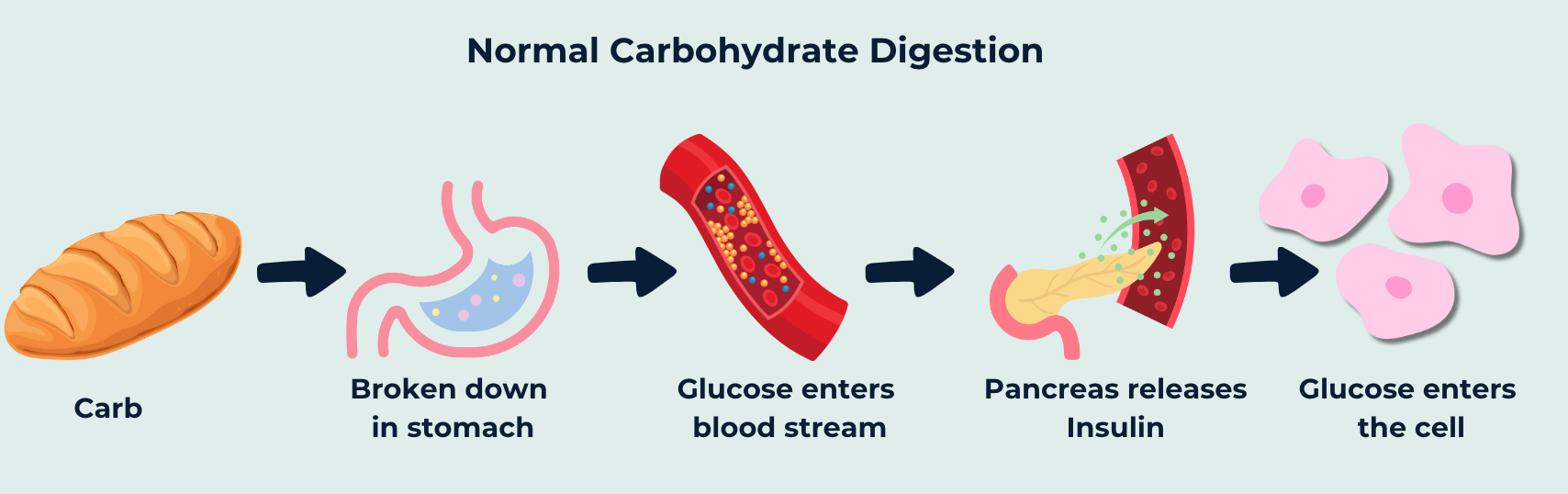
When we eat carbohydrates, they’re broken down into glucose- our body’s primary source of energy. To help move glucose from the bloodstream into our cells, the hormone insulin plays a key role. In insulin resistance, however, the body’s cells don’t respond as effectively to insulin, making it harder for glucose to be absorbed and used. This can lead to higher blood sugar levels, feelings of fatigue, and the body producing more insulin to compensate. Over time, this imbalance can contribute to many of the common symptoms of PCOS.
How to Support PCOS with Gentle Nutrition
Incorporating nutrient-dense foods into your diet can play a key role in improving insulin resistance & PCOS symptoms. Improving insulin resistance can boost energy levels, support appetite regulation, and promote a more regular menstrual cycle, which may enhance fertility outcomes. There is not one specific dietary approach that is recommended for PCOS. Instead, recommendations can be tailored to suit your individual symptoms and lifestyle.
Before making any dietary changes to manage PCOS, it’s essential to have a healthy relationship with food and your body. If you have a history of dieting or disordered eating, intentional dietary changes may feel triggering, so it’s important to proceed with care.
Focusing on adding in nutrients to support PCOS rather than cutting out foods can help to normalise relationship with food.
1.Choose Low-GI Carbohydrates
Not all carbs are created equal. Low-GI (glycaemic index) carbs release energy more slowly, helping to balance blood sugar levels and reduce insulin resistance.
Our favourite sources of Low-GI carbs include:
Rolled oats, basmati rice, lentils, pasta
Wholegrain bread, sourdough, sweet potato, corn
Milk, yogurt, wholegrain crispbread
2. Space Carbs Throughout the Day
Eating carbohydrates throughout the day in regular meals and snacks (rather than saving them for one big meal) can help manage blood glucose levels.
Eating regularly will also help to:
Stabilise energy and mood
Reduce cravings and binges
Improve hunger and fullness signals
Aim for 3 meals and 2-3 snacks across the day! In contrast, consuming just 2-3 larger meals with long gaps in between can lead to blood sugar spikes and crashes.
3. Include Healthy Fats
Fats are an essential part of our diet, however, reducing total fat intake and prioritising the replacement of saturated fats with monounsaturated and polyunsaturated fats can support cholesterol and triglyceride management, ultimately decreasing the risk of cardiovascular disease.
Sources of mono & poly unsaturated fats (the ones we want more of) include:
Avocado, olive oil, nuts and seeds
Fatty fish like salmon, sardines and mackerel
4. Focus on Fibre
Fibre helps slow glucose absorption- assisting insulin resistance, as well supporting digestion, and reducing cholesterol. Fibre is found in:
Whole grains like oats, wholegrain bread, brown rice
Legumes, nuts, seeds
Fruits and vegetables (especially with the skin on)
5. Move in a Way That Feels Good
Movement can help improve insulin resistance & hormone levels. Any movement is positive, and movement you enjoy is going to be more sustainable. These benefits are present regardless of changes in body shape or size. If you choose to have a higher GI meal, or consume a larger amount of carbohydrate than you usually would, it can help to move after your meal to lower BGLs.
Supportive movement might look like:
Walking
Yoga or stretching
Dancing or strength training
6. Include A Variety Of Fruits & Vegetables
Including a variety of different coloured fruits and vegetables can provide us with antioxidants. Antioxidants can help to reduce inflammation which can assist symptom management & can protect against the development of certain diseases.
Key Takeaways for Eating with PCOS
Focus on Low-GI carbohydrates spaced throughout the day
Replace saturated sources of fat with poly and mono unsaturated fats to protect cholesterol levels
Include sources of fibre daily for gut health & to slow down digestion
Move your body in a way you enjoy to support hormone & blood glucose levels
Eat regularly to stabilise BGLs, energy and honour hunger cues
Include a variety of different coloured fruits and vegetables for antioxidants
It's important to remember that even with nutrition and lifestyle changes, medication may still be part of your care. This isn’t a sign of failure it’s a reflection of the incredible advances in modern medicine that help manage risks and support better health outcomes.
There’s no one-size-fits-all approach to eating for PCOS. Managing symptoms isn’t about doing everything perfectly. Gently incorporating one or two supportive changes at a time can help create sustainable shifts over the long term. Not every strategy will suit every person, and that’s completely okay. The most important thing is to work with what feels right for you, your body, and your unique symptoms.
Looking for personalised support with PCOS?
Our team of non-diet dietitians are here to support you with compassion & evidence-based guidance. Whether you're navigating a new diagnosis, managing long-term symptoms, or exploring a gentler way to nourish your body- we’re here to help. Click here to get started today.